Arrival in Beijing, China for 100th Year Centenary Celebrations at Peking University
I just arrived in Beijing, China at the Beijing Airport and I wanted to share some of my pictures from my journey to the Peking University’s 100th Year Centenary Celebration that will include a dinner gala and forum presentations from university leaders from around the world. Here are some views from the Beijing Airport in Beijing, China.
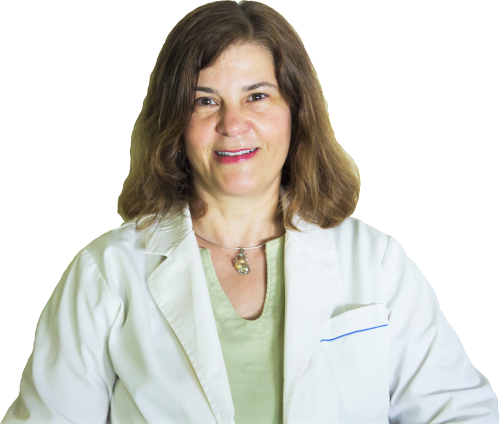
This is me standing in front of the Pathology Building at Peking University in Beijing, China.
This picture is me standing in front of the building that says Central Laboratory Tower with a classmate from Uganda and Nepal. The second picture is in front of a VIP parking for the 100 year anniversary celebration.
This is me with my two classmates in front of the Health Science Library. Andrew is from Uganda and practices orthopedic surgery in South Africa and Urmila is from Nepal where she is a Pediatric Cardiologist.
|
||||
Centenary Celebration and Gala Dinner at the International Center
The Centenary Celebration and Gala Dinner took place at the Conference Center at Peking University, Beijing, China, October 25, 2012.
There were representatives from All Chinese Medical Universities who delivered speeches, and to my surprise, the Dean from the University of Michigan Medical School, Dr. James O. Woolliscroft, also delivered a congratulation speech. Other speakers represented the University of Whales Medical School and Hong Kong as well as the Karolinska Institute from Sweden. Look how decorated the tables were. They also had wine and drinks which made it very nice.
The food included nicely decorated hors d’oeuvres and many, many dishes. Here’s my name tag as each seat at the table was reserved with each attendee’s name.
This last picture was taken in front of the stage were the speeches were delivered.
|
||||
Beijing University Health Science Center Centenary Celebration – The President and Dean’s Forum
There were many participants at The President and Dean’s forum at Peking University Health Science Center. Different universities participated from around the world including Yale, Pittsburgh, Michigan, Nebraska, and UCLA. Collaboration of medical education in China was one of the first topics by a representative from the Australian University. She talked about wisdom according to the ancient philosopher, Confucius, and how much is to be learned from the Chinese both in the ancient world and in the modern era. Their university has already established a program of exchange students and looking for further collaboration in many areas. The last photo is a slide of a key note speaker from UCLA integrating the Chinese symbol in his presentation I found it unusual and intresting. Saturday I am going to visit the Third Teaching Hospital where I did a part of my clinical training and see the changes that have taken place since I was there 5 years ago. Topics discussed at the President and Dean’s Forum 1. Essential Health Profrssionals for a China Century by Prof. Lincoln Chen, President,china Medical Board |
||||
LifeVantage Protandim
Protandim is a daily dietary supplement that is meant to help the body regulate cells to fight against aging. It does this by targeting a specific gene that keeps cells from oxidating, much like an anti-oxidant. It contains anti-inflammatory ingredients such as turmeric extract along with green tea extract, milk thistle extract, among others. Protandim is the only supplement on the market clinically proven to reduce oxidative stress which slows down the cell aging process. This is not a conventional antioxidant supplement. Each caplet contains photonutrients that tell the body’s genes to produce it’s own antioxidant enzymes. This increases the antioxidant power more than any other conventional supplement or food. Protandim is 100% Vegetarian – Free of Gluten, Wheat, Dairy, Gelatin and Yeast. Everyone in the Kokkalis family enjoys using Protandim. My sons take it because they are playing soccer and are prone to tissue damage from a high contact sport. I enjoy taking it to help me stay young and healthy! |
||||
Beijing Medical University Celebrates 100 Years
Dr. Angelica Kokkalis Plans to Attend 100 Year Celebration in China In 1998 Beijing University celebrated it’s 100 year anniversary and this October 2012, Beijing Medical University will celebrate it’s 100 year anniversary. Dr. Angelica Kokkalis, Indianapolis acupuncture and Eastern medicine doctor, is planning to go to China for two weeks to attend the celebrations. Dr. Kokkalis was invited to give a talk as one of the first foreign student medical graduates and she hopes she can collaborate with the university doing some research on the effects of acupuncture and autism. The department of Neuroscience and the leading world renown prof Ji Sheng Han have already great results from preliminary studies. About Beijing Medical University (now called Peking University Health Science Center) Established by the central government of China on October 26, 1912 in the city of Beijing, Beijing Medical University was the first of the kind in China to teach western medicine and train medical professionals. In 1923 it adopted the name Beijing Medical University, but in the year 2000 it merged with Peking University and is now named Peking University Health Science Center.
According to Wikipedia, “PUHSC offers a full range of courses for 8 specialties including basic medical sciences, clinical medicine, preventive medicine, stomatology, pharmacy, nursing, medical laboratory diagnosis and biomedical English. It has 57 accredited doctoral programs and 66 master programs. In addition to offering undergraduate and graduate programs, it also plays an active role in continuing education. PUHSC hosts 6 postdoctoral programs. PUHSC now has enrollment of 10112 students, including 927 doctoral students, 1036 master program students, 3196 undergraduates, 696 junior college students, 3994 adult learning program students, and 388 international students. It has many international students. PUHSC has developed 20 disciplines that have gained national recognition. Besides, it has 1 national key laboratory, 10 ministry-level key laboratories, 23 joint research centers, and 20 research institutes at university level. PUHSC has 11 schools, 1 institute and 1 division, namely, School of Basic Medical Sciences, School of Pharmaceutical Sciences, School of Public Health, School of Nursing, School of Stomatology, the First School of Clinical Medicine (Beida Hospital), the Second School of Clinical Medicine(the people’s Hospital), the Third School of Clinical Medicine (the Third Hospital), Institute of Mental Health (the Sixth Hospital), the School of Oncology (Beijing Tumor Hospital), Peking University Shenzhen School of Medicine, Peking University School of Telemedical Education, and the Division of Humanity and Fundamental Sciences. In addition, 15 hospitals in Beijing serve as teaching hospital.” |