Angelica Kokkalis recently attended Signature HealthCARE of Lafayette’s wellness far. She was super excited about the wellness event that happened, Wednesday, June 17th, 2015 at Signature HealthCARE of Lafayette.
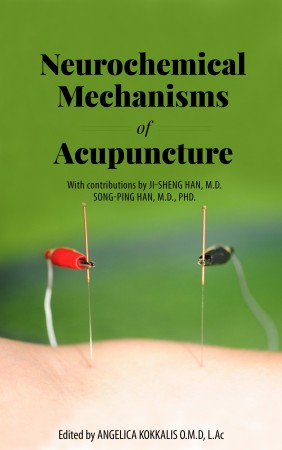 In Neurochemical Mechanisms of Acupuncture, writers Dr. Song-Ping Han and Dr. Ji-Sheng Han present the first book of a collection of studies on the neurochemical mechanisms of acupuncture that have been conducted by Dr. Ji-Sheng Han and his associates at Beijing Medical University This alternative therapy with its 3,500 year old history, is now gaining credibility and respect. The authors offer a unique blend of knowledge having a combined clinical and research acupuncture experience of over 70 years.
In Neurochemical Mechanisms of Acupuncture, writers Dr. Song-Ping Han and Dr. Ji-Sheng Han present the first book of a collection of studies on the neurochemical mechanisms of acupuncture that have been conducted by Dr. Ji-Sheng Han and his associates at Beijing Medical University This alternative therapy with its 3,500 year old history, is now gaining credibility and respect. The authors offer a unique blend of knowledge having a combined clinical and research acupuncture experience of over 70 years.
This book is a scientifically supported explanation of the basic neurochemical mechanisms and processes underlying the practice of acupuncture. This may well be one of the most valuable books of acupuncture you will ever read. It is also a teaching manual by which an evidence based, highly effective no-drug method of treatment can be used to treat pain, psychiatric and other chronic illnesses.
This is a book that belongs in the library of every physician, medical school and school of Chinese medicine. Several other studies of Dr. Ji-Sheng Han will be introduced in subsequence to this book including his recent research in the considerable successful treatment of autism and assisted reproductive medicine.
“A compilation of a leading researcher’s work, in any field, would be an excellent single point of reference for future generations to build upon. In order to accelerate progress, knowledge of what has already been discovered is of the utmost importance and would be invaluable to current researchers and practitioners if this knowledge were compiled into a life-work compilation.” -Cari Skaggs, Philosopher
Dr. Angelica D. Kokkalis is the editor and President of the Han Institute. She is a graduate of Beijing Medical University class of 1989 and currently resides in Indiana USA.
Dr. Angelica Kokkalis will be attending the Pacific Symposium in San Diego, California this November 4-11, 2014. It is an opportunity for her to experience a community of healers while learning from innovators in the field. It will showcase 73 exhibitors eager to present new products that can help you and your health.
This event draws acupuncturists, massage practitioners, chiropractors, nurses, medical doctors and traditional Chinese medicine students from all over the country. She will earn continuing education credits while listening to this year’s speakers present current research, unique methodologies, and explore new techniques to integrate into your daily practice.
Since 1987, this event has served as an interactive environment for brilliant minds of the Eastern medical profession to come together and thrive. A renowned conference with worldwide recognition, this annual event unites acupuncturists, massage therapists, students, and professors by opening the gates to the exchange of industry information.
Research shows that soldiers with post-traumatic stress disorder (PTSD) given hypnotherapy treatment while using electro-acupuncture for 30 minutes at the same time can be useful in alleviating the symptoms these patients experience (Ref.1) and is twice as effective as traditional acupuncture. A recent PTSD study on the effects of electro-acupuncture confirms this.
What is Electro-Acupuncture?
Electro-acupuncture is a complementary medical treatment that has been authorized by the FDA. It uses electrically-conducting polymer pads or EKG pads instead of traditional acupuncture needles. Not only is this method needle free, but the weak electrical impulses that are used with electro-acupuncture treatment double the effectiveness of the older acupuncture method.
History of Electro-Acupuncture
Professor Ji-Sheng Han from the Beijing Medical University conducted systematic experiments to study the phenomenon of electro-acupuncture (Ref. 2). Dr. Han did 30 years of experimentation and also observed patients very closely. He explained that traditional Chinese acupuncture points were merely spots on the body where electric currents are picked up easier and transmitted to the brain.
1: George A. Ulett, M.D., Ph.D. and SongPing Han, B.M., Ph.D.: “The Biology of Acupuncture”, copyright 2002, Warren H. Green Inc., Saint Louis, Missouri, 63132 USA
2. J.S. Han: “The Neurochemical Basis of Pain Relief by Acupuncture”. Vol. 2. Hu Bei Science and Technology Press, Beijing, 1998 (784 pages).
Dr. Angelica Kokkalis Plans to Attend 100 Year Celebration in China
In 1998 Beijing University celebrated it’s 100 year anniversary and this October 2012, Beijing Medical University will celebrate it’s 100 year anniversary. Dr. Angelica Kokkalis, Indianapolis acupuncture and Eastern medicine doctor, is planning to go to China for two weeks to attend the celebrations.
Dr. Kokkalis was invited to give a talk as one of the first foreign student medical graduates and she hopes she can collaborate with the university doing some research on the effects of acupuncture and autism. The department of Neuroscience and the leading world renown prof Ji Sheng Han have already great results from preliminary studies.
About Beijing Medical University (now called Peking University Health Science Center)
Established by the central government of China on October 26, 1912 in the city of Beijing, Beijing Medical University was the first of the kind in China to teach western medicine and train medical professionals. In 1923 it adopted the name Beijing Medical University, but in the year 2000 it merged with Peking University and is now named Peking University Health Science Center.

According to Wikipedia, “PUHSC offers a full range of courses for 8 specialties including basic medical sciences, clinical medicine, preventive medicine, stomatology, pharmacy, nursing, medical laboratory diagnosis and biomedical English. It has 57 accredited doctoral programs and 66 master programs. In addition to offering undergraduate and graduate programs, it also plays an active role in continuing education. PUHSC hosts 6 postdoctoral programs. PUHSC now has enrollment of 10112 students, including 927 doctoral students, 1036 master program students, 3196 undergraduates, 696 junior college students, 3994 adult learning program students, and 388 international students. It has many international students.
PUHSC has developed 20 disciplines that have gained national recognition. Besides, it has 1 national key laboratory, 10 ministry-level key laboratories, 23 joint research centers, and 20 research institutes at university level. PUHSC has 11 schools, 1 institute and 1 division, namely, School of Basic Medical Sciences, School of Pharmaceutical Sciences, School of Public Health, School of Nursing, School of Stomatology, the First School of Clinical Medicine (Beida Hospital), the Second School of Clinical Medicine(the people’s Hospital), the Third School of Clinical Medicine (the Third Hospital), Institute of Mental Health (the Sixth Hospital), the School of Oncology (Beijing Tumor Hospital), Peking University Shenzhen School of Medicine, Peking University School of Telemedical Education, and the Division of Humanity and Fundamental Sciences. In addition, 15 hospitals in Beijing serve as teaching hospital.”